The Intent of an AI Discharge Summary Agent
Hospital discharge notes contain critical patient information, but when received as faxes, they often create bottlenecks in clinical workflows. Physicians must wade through dense, multi-page documents to extract key clinical details. An AI-powered fax summarization system aims to transform this process by automatically identifying and highlighting critical information, enabling physicians to quickly grasp essential patient data while maintaining access to the complete document when needed.
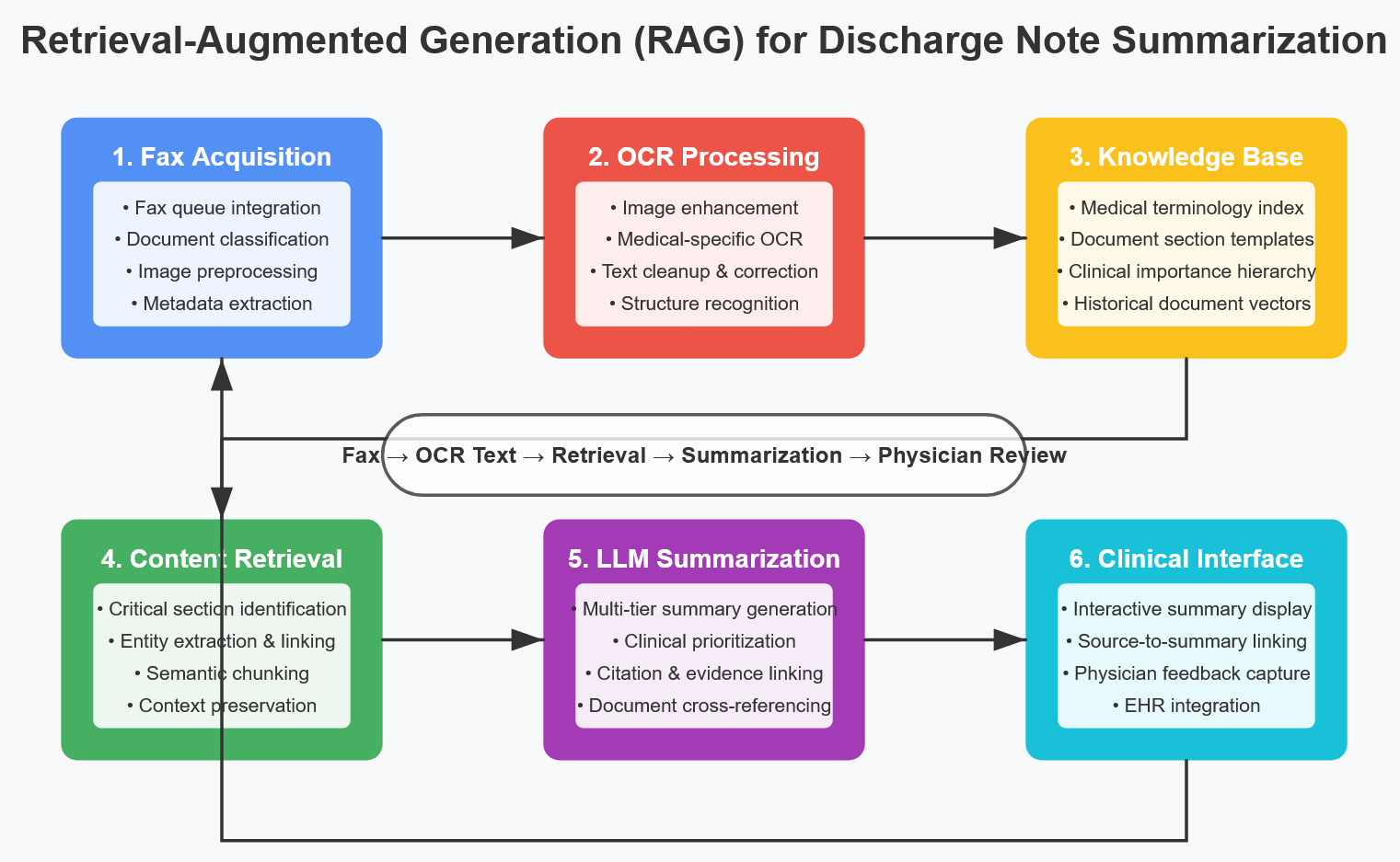
Building the Foundation: System Architecture and Data Requirements
Fax Queue Integration
The first step involves establishing a secure connection to the existing fax queue system:
- API Integration: Connect to existing digital fax platforms through their APIs
- SFTP/Secure Email: Set up automated retrieval for systems using SFTP or email
- Direct HL7 Feeds: For health systems with integrated EHRs, establish direct HL7 interfaces
- Document Management: Create a repository for incoming faxes with appropriate metadata
OCR Processing Pipeline
Converting fax images to machine-readable text requires a robust OCR pipeline:
- Image Preprocessing:
- Image enhancement (contrast adjustment, noise reduction)
- Deskewing and rotation correction
- Removal of artifacts and non-text elements
- Resolution standardization
- OCR Engine Selection:
- Commercial solutions (ABBYY FineReader, Adobe Document Cloud)
- Open-source options (Tesseract, EasyOCR)
- Cloud services (Google Document AI, AWS Textract, Azure Form Recognizer)
- Medical-Specific OCR Optimizations:
- Medical terminology dictionaries for improved recognition
- Template matching for common discharge note formats
- Context-aware correction for medical terms and measurements
- Table and structured data recognition
Training Data Requirements
Building an effective summarization model requires comprehensive training data:
- Discharge Note Corpus:
- Collect 1,000+ anonymized discharge summaries
- Ensure diversity across specialties, hospitals, and formats
- Include variations in quality (clean electronic documents vs. poor fax quality)
- Expert Annotations:
- Physician-annotated highlights of critical information
- Categorization of content (medications, follow-up instructions, diagnoses)
- Priority ratings for different information types
- Cross-physician agreement scoring
- Document Structure Dataset:
- Maps of common discharge summary formats and section headings
- Section importance hierarchies for different clinical contexts
- Specialty-specific section relevance ratings
Development Process: Building the AI Summarization Engine
NLP Preprocessing
Before LLM processing, establish an effective text preparation pipeline:
- Text Cleanup:
- Remove artifacts from OCR process (stray characters, header/footer remnants)
- Standardize formatting (spacing, line breaks, bullet points)
- Normalize medical terminology and abbreviations
- Document Segmentation:
- Identify and tag document sections
- Recognize headers, subheaders, and organizational elements
- Separate narrative text from structured data (tables, lists)
- Entity Recognition:
- Identify key medical entities (medications, dosages, diagnoses)
- Extract dates, times, and temporal relationships
- Recognize healthcare provider names and specialties
- Identify facility and contact information
LLM Model Selection and Tuning
Choosing the right foundation model is critical:
- Model Selection Criteria:
- Medical knowledge capabilities
- Context window sufficient for long documents
- Fine-tuning capabilities
- Deployment requirements (on-premises vs. cloud)
- Fine-tuning Approaches:
- Domain adaptation using medical literature
- Task-specific tuning with annotated discharge summaries
- Few-shot learning with exemplar summaries
- RLHF using physician feedback
- Prompt Engineering:
- Develop structured prompting templates for consistent results
- Include explicit instructions for information hierarchy
- Implement specialty-specific prompting variations
- Create fallback prompting strategies for complex documents
Summarization Strategy
Develop a multi-layered approach to summarization:
- Tiered Summary Structure:
- Ultra-concise overview (5-7 bullet points)
- Section-by-section key points
- Detailed extraction of critical elements
- Information Prioritization:
- New diagnoses and findings
- Medication changes (additions, discontinuations, dosage adjustments)
- Required follow-up actions and appointments
- Critical test results and pending studies
- Care transition requirements
- Visual Enhancement:
- Color-coding by information type or urgency
- Progressive disclosure interfaces
- Comparison highlighting for changed elements
- Timeline visualization for sequential events
Document Linking and Navigation
Create seamless connections between summary and source:
- Bi-directional Linking:
- Map each summary point to original document location
- Enable click-through from summary to source context
- Provide context window showing surrounding text
- Visual Navigation:
- Document thumbnails with highlighted regions
- Mini-map navigation for long documents
- Heat map visualization of information density
- Search Integration:
- Full-text search across original document
- Entity-based filtering
- Semantic search capabilities
Testing and Validation
Implement rigorous validation to ensure clinical safety and effectiveness:
Technical Validation
- OCR Accuracy Testing:
- Character and word-level accuracy metrics
- Special focus on numerical data and medication names
- Performance across varying document qualities
- Table and structured data extraction accuracy
- Summarization Quality Metrics:
- ROUGE and BLEU scores against physician-created summaries
- Critical information inclusion rate
- False positive/negative rates for key medical facts
- Consistency across similar documents
Clinical Validation
- Physician Review Protocols:
- Blinded comparisons of AI vs. human summaries
- Time-to-comprehension measurements
- Critical information identification tests
- User experience and cognitive load assessment
- Workflow Integration Testing:
- Time savings measurements
- Click/interaction analysis
- Error rates in subsequent clinical documentation
- Impact on clinical decision-making
- Safety Monitoring:
- Missing critical information tracking
- Misleading summary identification
- Edge case detection and handling
- Recovery mechanisms for system failures
Iteration and Refinement
Establish continuous improvement processes:
Feedback Collection
- Structured Feedback Channels:
- In-app rating and feedback mechanisms
- Periodic user surveys
- Focus group sessions with clinical users
- Automated tracking of summary modifications
- Error Analysis:
- Categorization of error types
- Root cause analysis for systematic failures
- Correlation with document characteristics
- Specialty-specific issue identification
Model Refinement
- Targeted Retraining:
- Expand training data in problematic areas
- Adjust prompting strategies for identified weaknesses
- Implement specialized models for challenging document types
- Deploy continuous learning from physician corrections
- Feature Enhancement:
- Develop specialty-specific summarization modes
- Implement user preference customization
- Create adaptive interfaces based on usage patterns
- Add cross-document patient history integration
Implementation Case Study: Primary Care Practice
A 10-physician primary care practice implemented the AI discharge summary system with these results:
- Before Implementation:
- Average 8.5 minutes spent reviewing each discharge summary
- 24-hour average lag between receipt and review
- 15% rate of missed follow-up items
- High physician dissatisfaction with fax workflow
- After Implementation:
- Average 2.3 minutes spent reviewing each discharge summary
- Same-day review rate increased from 45% to 92%
- Missed follow-up items decreased to 3%
- 87% of physicians reported reduced cognitive burden
Conclusion
AI-powered discharge note summarization represents a transformative approach to clinical documentation workflows. By combining OCR technology, advanced NLP, and physician-centered design, these systems can dramatically reduce the time and cognitive load associated with reviewing faxed clinical documents.
The most effective implementations maintain a careful balance between automation and physician oversight, ensuring that AI augments rather than replaces clinical judgment. By providing concise, prioritized information with seamless access to source documentation, these systems help physicians focus on patient care rather than paperwork navigation.
As healthcare continues to struggle with interoperability challenges, intelligent document processing systems serve as a practical bridge between disparate systems, bringing the benefits of structured data even to information trapped in faxed documents. The result is more efficient workflows, better care coordination, and ultimately improved patient outcomes.
