The Intent of an AI Appointment Management Agent
Healthcare providers lose billions annually due to appointment no-shows. Beyond financial impacts, no-shows disrupt schedules, waste valuable clinical time, and prevent other patients from receiving timely care. An AI appointment management agent aims to identify patients at high risk of missing appointments and enable strategic double-booking to maximize clinic efficiency without compromising patient experience.
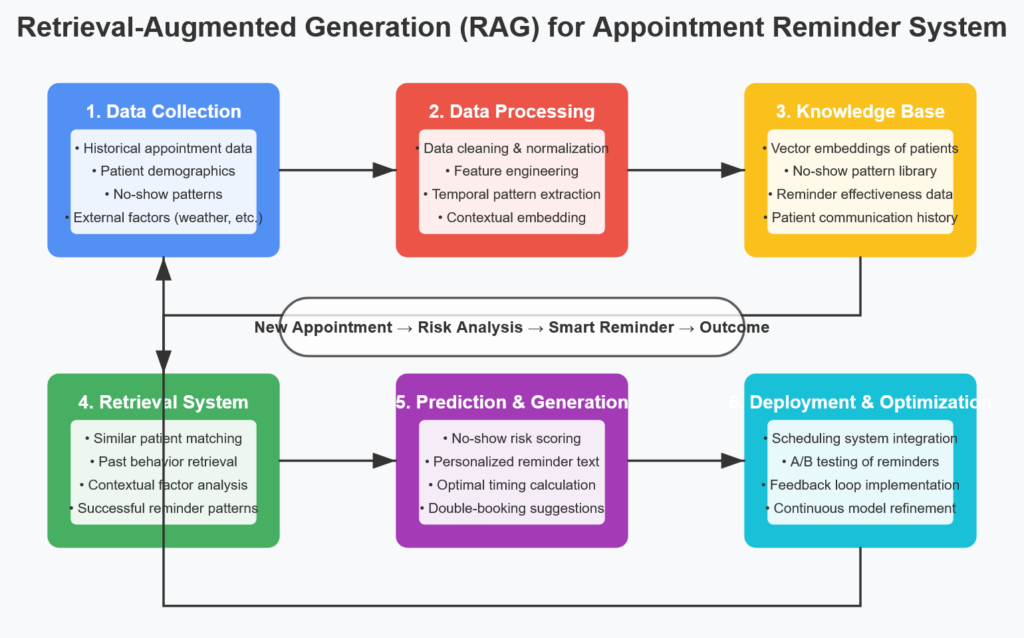
Building the Foundation: Data Collection and Preparation
The quality of your AI no-show prediction system hinges on comprehensive, accurate data. Here’s how to build a solid data foundation:
Historical Appointment Data
Start by collecting at least 12-18 months of historical appointment data, including:
- Demographic information (age, gender, insurance type)
- Appointment details (date, time, day of week, provider, specialty)
- Lead time (days between scheduling and appointment)
- Patient history (previous no-shows, cancellations, reschedulings)
- Weather conditions on appointment days
- Transportation factors (distance from clinic, public transit access)
- Communication records (reminder responses, confirmation rates)
Data Preparation and Cleansing
Raw healthcare data requires significant preparation:
- Address missing values: Implement strategies for handling incomplete records without introducing bias
- Normalize data: Convert categorical variables into numerical representations
- Balance the dataset: Address potential imbalances between no-show and attended appointments
- Feature engineering: Create derived variables like “days since last appointment” or “historical no-show rate”
- Data labeling: Clearly define what constitutes a “no-show” versus late cancellations
Privacy and Compliance
All data handling must adhere to:
- HIPAA requirements for protected health information (PHI)
- Relevant state and local healthcare privacy regulations
- Ethical considerations for using patient data in predictive models
Developing the Predictive Model
With clean, comprehensive data in place, we can develop the AI model:
Model Selection
Several machine learning approaches work well for no-show prediction:
- Gradient Boosting Models: XGBoost and LightGBM excel at handling mixed data types and capturing non-linear relationships
- Random Forests: Provide good interpretability while handling complex patterns
- Neural Networks: Can capture nuanced relationships but require larger datasets
- Logistic Regression: Offers high interpretability for simpler implementations
Feature Importance Analysis
Understanding which factors most strongly predict no-shows helps both model development and practical interventions:
Top Predictive Factors (Example):
- Previous no-show history (41% importance)
- Lead time between booking and appointment (22%)
- Day of week (11%)
- Patient age (8%)
- Insurance type (7%)
- Appointment time (6%)
- Weather forecast (3%)
- Provider specialty (2%)
Risk Scoring System
Rather than binary classification, develop a risk score from 0-100 that allows for tiered interventions:
- High risk (80-100): Strategic double-booking candidates
- Medium risk (40-79): Enhanced reminder protocols
- Low risk (0-39): Standard reminder procedures
Testing and Validation
Rigorous testing ensures your AI system makes reliable predictions before deployment:
Evaluation Metrics
Focus on these key performance indicators:
- True positive rate: Correctly identified no-shows
- False positive rate: Patients incorrectly flagged as likely no-shows
- Area Under the ROC Curve (AUC): Overall model discriminative ability
- Precision and Recall: Balance between correct identification and comprehensive coverage
- Financial impact metrics: Projected revenue saved vs. intervention costs
Validation Approaches
Implement these validation strategies:
- Cross-validation: Test on multiple random data subsets
- Temporal validation: Test on future time periods to simulate real-world implementation
- Shadow deployment: Run the system alongside existing processes to compare outcomes without acting on predictions
- A/B testing: Apply interventions to a subset of patients to evaluate effectiveness
Implementation and Workflow Integration
A successful AI appointment system must integrate seamlessly with existing clinical workflows:
The Double-Booking Strategy
For high-risk appointments:
- Selective double-booking: Only double-book slots with patients flagged as high-risk (80+ risk score)
- Provider-specific policies: Adjust double-booking thresholds based on provider preference and specialty
- Time buffers: Schedule high-risk appointments at the beginning of sessions or before natural breaks
- Resource planning: Ensure adequate staffing when double-booked slots are scheduled
Tiered Intervention System
Based on risk scores, implement escalating interventions:
- Low risk (0-39): Standard SMS reminder 48 hours before appointment
- Medium risk (40-79): SMS + phone call reminder, offer transportation assistance
- High risk (80-100): Personal call from clinical staff, confirmation requirement, double-booking consideration
Staff Training
Prepare your team to work with the AI-powered system:
- Train front desk staff to interpret risk scores
- Develop clear protocols for double-booking decisions
- Create scripts for different intervention levels
- Establish procedures for handling patient questions about the system
Continuous Improvement
The AI appointment system should evolve over time:
Performance Monitoring
Track these metrics continuously:
- No-show rate compared to baseline
- Double-booking utilization and outcomes
- Provider and staff satisfaction
- Patient feedback and complaints
- Financial impact (revenue increase, cost savings)
Model Retraining
Schedule regular model updates:
- Retrain quarterly with new appointment data
- Adjust for seasonal variations
- Update for demographic shifts in patient population
- Incorporate new features as data becomes available
Ethical Considerations
Address these ongoing concerns:
- Monitor for bias across demographic groups
- Ensure interventions don’t disproportionately impact vulnerable populations
- Maintain transparency with patients about how scheduling decisions are made
- Regularly review HIPAA compliance as the system evolves
Results and Impact
When properly implemented, AI-powered appointment systems typically deliver:
- 25-35% reduction in overall no-show rates
- 15-20% increase in provider utilization
- $20,000-$30,000 annual revenue increase per provider
- Improved patient access to care through optimized scheduling
- Reduced wait times for appointments
- Higher patient satisfaction scores
Conclusion
AI-powered appointment management represents a major advancement in healthcare operations. By predicting no-shows and enabling strategic double-booking, these systems recover lost revenue, improve provider productivity, and ultimately enhance patient access to care.
The most successful implementations combine sophisticated predictive modeling with thoughtful human oversight and patient-centered communication strategies. When technology and human expertise work together, the result is a more efficient practice that better serves both providers and patients.
